Traditional semen analysis, a standard since the 1950s, often leaves couples with unanswered questions – 25-30% of infertility cases remain unexplained.
Enter Sperm DNA Fragmentation (SDF) – a ground-breaking biomarker that goes beyond basic sperm counts to uncover hidden damage linked to infertility, failed IVF treatments, and recurrent miscarriages. Let’s explore why SDF testing is transforming male fertility diagnostics.
Sperm DNA fragmentation testing is now recognised as an important part of fertility assessments and is increasingly recommended by leading organisations worldwide.
These guidelines emphasise the critical role of SDF testing in improving clinical decision-making and fertility treatment outcomes.
- World Health Organization (WHO): Includes SDF testing in its 2021 extended examination list.
- European Association of Urology (EAU): Recommends SDF testing for couples with recurrent pregnancy loss (RPL) from natural conception, failure of assisted reproductive technology (ART), or men with unexplained infertility1.
- Global Andrology Forum (GAF): Highlights SDF testing for unexplained and idiopathic male infertility, recurrent miscarriage, clinical varicocele, and ART failure, including recurrent implantation or fertilisation failure2.
Research Findings
SDF: A Hidden Factor in Male Infertility
Traditional semen analysis focuses on sperm count and motility but overlooks the genetic quality of sperm.
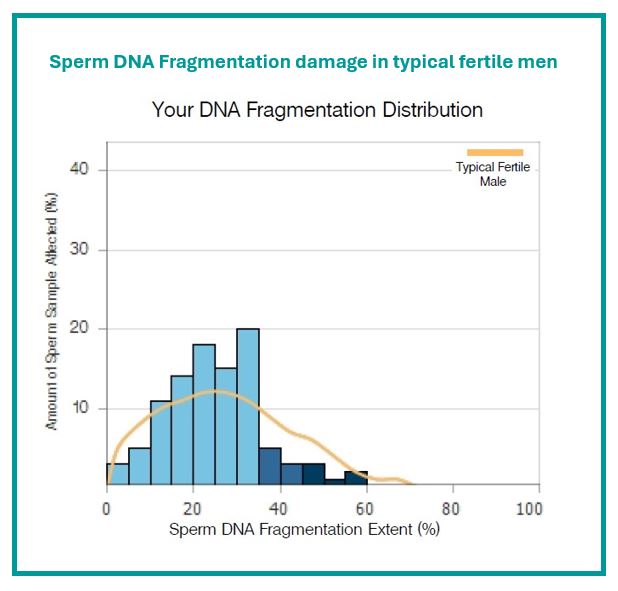
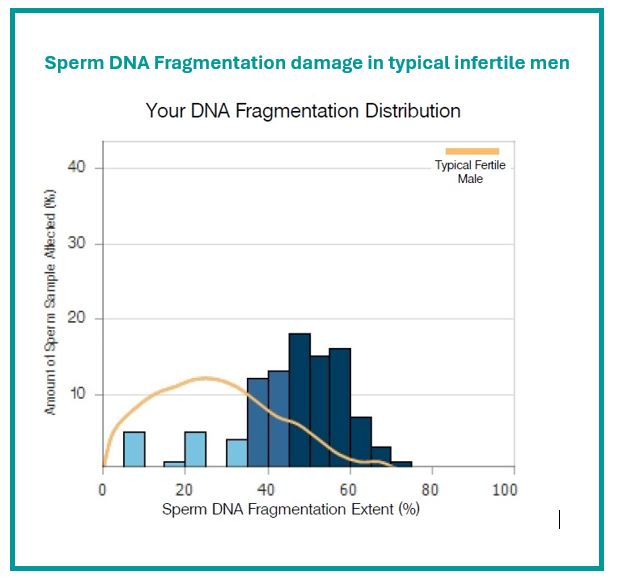
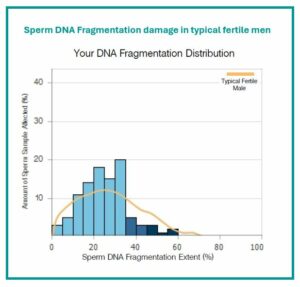
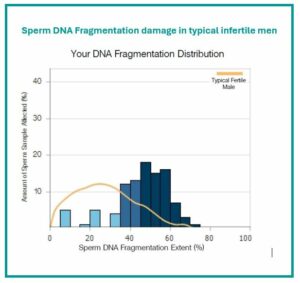
Examen research has shown that sperm from fertile men have low levels of DNA fragmentation compared to sperm from infertile men (Figures 1 and 2).
By identifying DNA damage, SDF testing provides actionable insights that can guide effective fertility treatments.
Scientific References – SDF & Infertility
SDF & IVF Live Birth Outcomes
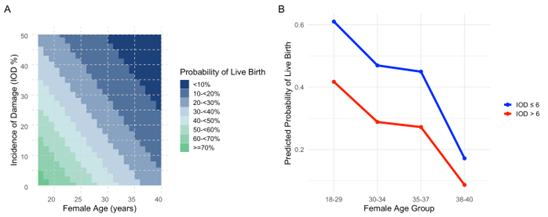
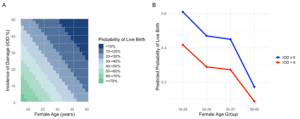
Based on Examen research, increased levels of double-stranded DNA fragmentation result in a lower likelihood of a live birth outcome following IVF treatment (Figure 3a &b).
Examen’s Extend test identifies this critical factor, empowering couples and clinicians to choose the most effective treatment path.
Research also shows a strong correlation between SDF levels, female age, and IVF success – making SDF testing an essential tool for personalised fertility care.
Scientific References – SDF & Fertility Treatment Success
- A systematic review and meta‐analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome
- Double-Stranded Sperm DNA Fragmentation measured with Neutral Comet Assay as a Predictor of IVF Outcomes: Evidence from Three European Clinics in a Multi-Centred Prospective Study
- Sperm DNA damage has a negative association with live-birth rates after IVF
SDF & Recurrent Miscarriage
For the 1-2% of couples facing recurrent miscarriage, the cause often remains a mystery.
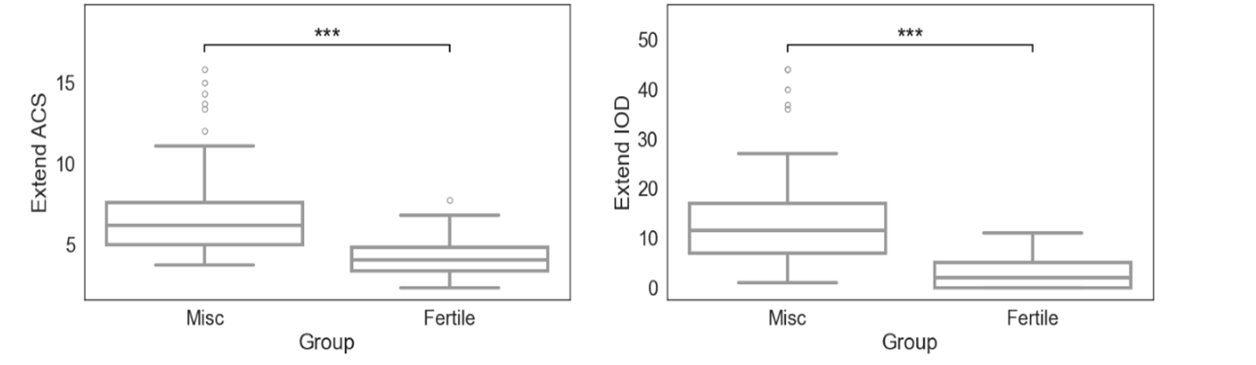
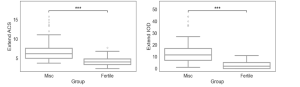
Examen’s research reveals that increased levels of double-stranded DNA fragmentation, as determined by the Extend test, were strongly associated with recurrent early pregnancy loss (Figure 4).
By identifying this hidden factor, SDF testing empowers couples with the knowledge to take proactive steps toward a successful pregnancy.
Scientific References – SDF & Recurrent Miscarriage
- Sperm DNA fragmentation is a novel biomarker for early pregnancy loss
- Sperm DNA fragmentation in Italian couples with recurrent pregnancy loss
- The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis
- Double-stranded sperm DNA fragmentation assessed using comet assay is associated with recurrent pregnancy loss
- Double Stranded Sperm DNA Breaks, Measured by Comet Assay, Are Associated with Unexplained Recurrent Miscarriage in Couples without a Female Factor
Join the leaders in fertility care
Our testing service can be set up within your own clinic, allowing your patients direct access to our market-leading Exact & Extend SDF tests, powered by SpermComet® technology.
We work closely with individual clinics to tailor our service to meet their needs.